Pasteur Eye Hospital
Eye Conditions
Contact Us
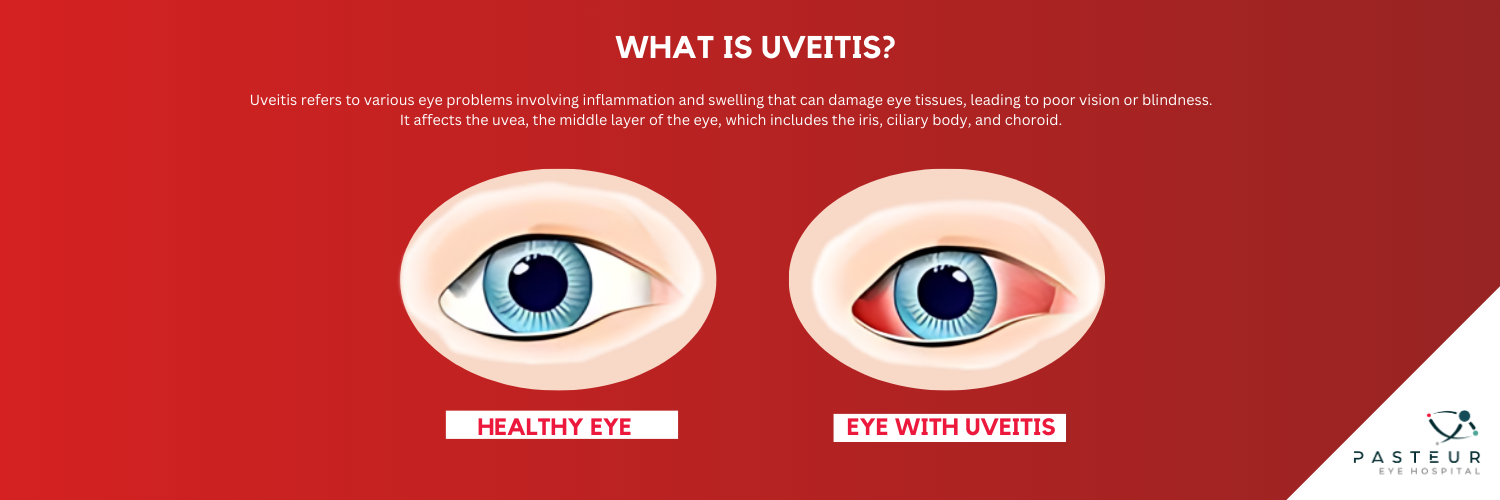
Uveitis is a broad term for various eye problems characterized by inflammation and swelling that can damage eye tissues, potentially leading to poor vision or blindness. The term “uveitis” is derived from the uvea, the middle layer of the eye that is most often affected by this condition. The uvea lies between the white part of the eye (sclera) and the inner layers. It contains three important structures: the iris, ciliary body, and choroid.
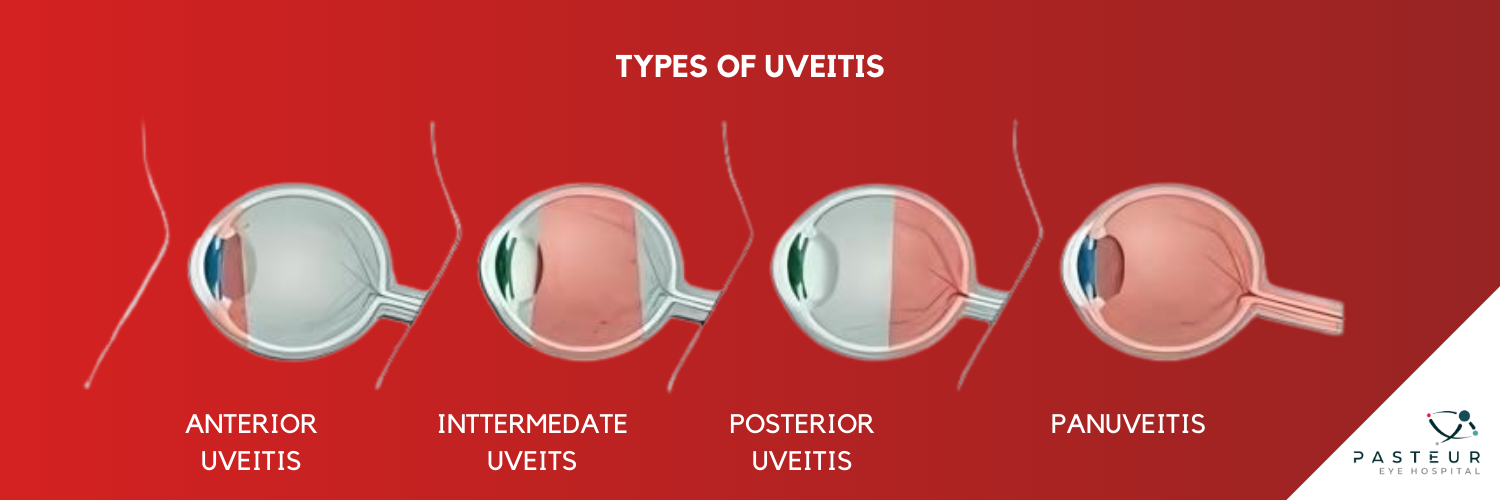
Yes, uveitis can be classified into different types based on the location of the inflammation:
Uveitis can be caused by various factors, all related to inflammation:
Certain individuals are at a higher risk of developing uveitis, including those with specific gene combinations and smokers. Various diseases also increase the likelihood of uveitis, such as:
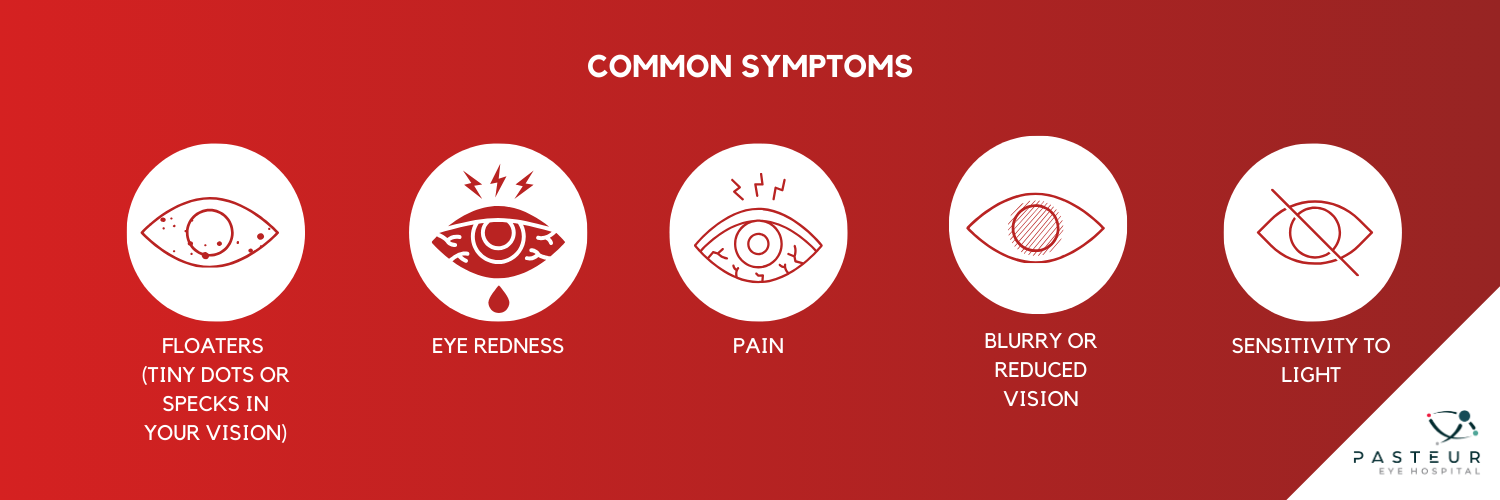
Symptoms of uveitis can affect one or both eyes and may appear suddenly or gradually. Warning signs include:
If you experience any of these symptoms, it’s crucial to see an eye doctor promptly to prevent serious complications.
Diagnosing uveitis involves a thorough eye exam and a review of your medical history and overall health. Additional tests such as blood tests, skin tests, or X-rays may be necessary to identify the underlying cause.
Treatment for uveitis aims to reduce inflammation and prevent further damage. Initial treatment may include corticosteroid eye drops. If these are ineffective, additional medications or injections may be required. For infections, antibiotics or antivirals are prescribed.
In severe cases, stronger drugs such as immunosuppressives may be necessary. Eye drops are commonly used for anterior uveitis, while intermediate, posterior, or panuveitis may require oral medications, injections, or an implantable device that releases medication slowly.
In some instances, a surgical procedure may be recommended to remove part of the vitreous (the gel-like substance in the eye).
Consistent follow-up with your doctor is essential to manage uveitis and prevent complications. Report any new symptoms immediately. Regular eye exams and maintaining overall health can help in early detection and management of uveitis.
Uveitis is a serious condition that requires prompt medical attention to protect your vision. If you have symptoms or are at risk, consult your eye doctor to discuss the best treatment options for you.
Pasteur Eye Hospital
Eye Conditions
Contact Us
© Copyright 2022 Pasteur Eye Hospital. All Rights Reserved.
No article or picture may be reproduced\published without the written consent of Pasteur Eye Hospital.
Managed with ❤️ by Cuberoo